Main Article – On precision prevention of melanoma

By Katie J. Lee and H. Peter Soyer
Katie J. Lee and H. Peter Soyer
The University of Queensland Diamantina Institute, The University of Queensland, Dermatology Research Centre, Brisbane, Australia.
Precision prevention of melanoma combines risk assessments based on personal and familial melanoma history, clinical phenotype, and genotype to stratify patients into a structured surveillance protocol, with more frequent surveillance for higher risk patients, and self-surveillance for low-risk patients. Surveillance is carried out with sequential 3D total body photography and dermoscopy, or mobile teledermoscopy for self-surveillance, and can be combined with telehealth for patients in regional and rural areas, for whom expert dermatological review is often out of reach.
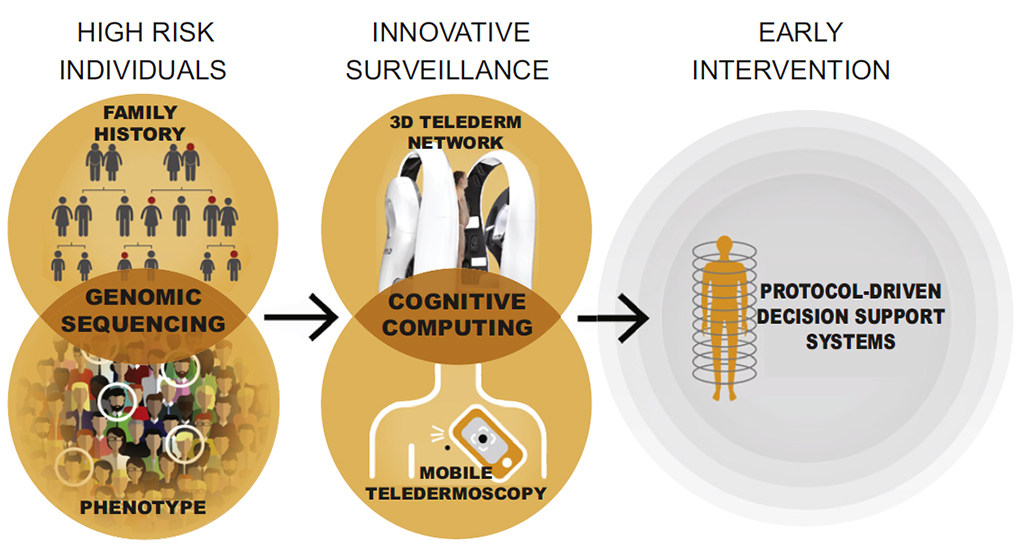
Figure 1. Precision prevention of melanoma involves a personalised approach to melanoma management, with risk stratification and innovative surveillance techniques.1
A key component of precision prevention is appropriate risk stratification, to allow patients to receive surveillance appropriate to their own situation rather than imposing a one-size-fits-all approach. Melanoma risk is influenced by a variety of genetic, familial and environmental inputs, and can be measured in a variety of ways, but for best results a holistic risk score needs to be developed. This includes clinical data and easily-observed phenotype traits, such as age, hair, eye and skin colour, and medical history; “deep” phenotype, referring to whole-body measures of naevi, freckling, and chronic UV photodamage, which can be extracted from total body 3D imaging via AI tools; and genotype, comprising high-penetrance familial melanoma genes and a polygenic risk score of all common point mutations (single nucleotide polymorphisms; SNPs) known to modify melanoma risk. Rare variant scores may also be added in future to detect patients who otherwise appear to be low risk.
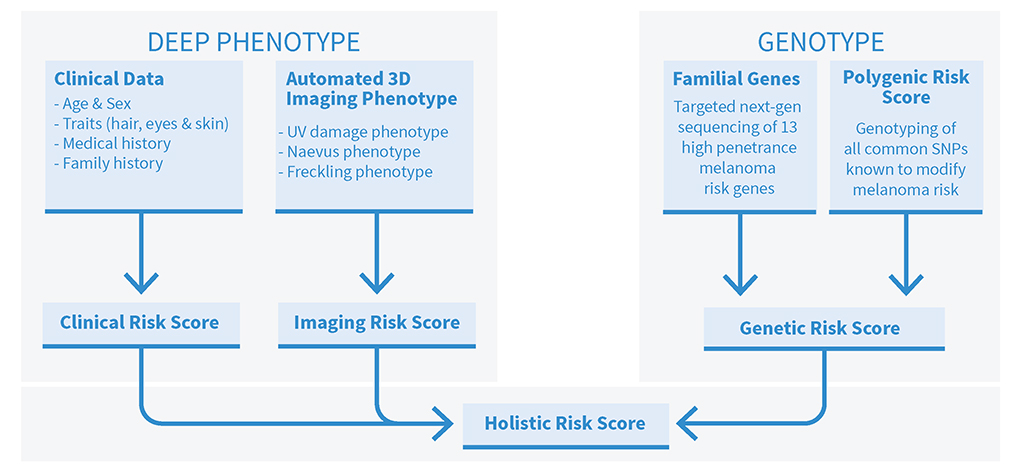
Figure 2. Elements of a holistic risk assessment. By generating a risk score for each patient, it is possible to divert each patient to a personally tailored schedule of screening to maximise early melanoma detection while minimising cost,
inconvenience to the patient, and excision of benign lesions. For high-risk patients, effective screening will increasingly rely on 3D whole body imaging systems, with AI clinical support tools and protocol-driven decision making. Low-risk patients can be educated to monitor their own skin, supported by mobile teledermoscopy or melanoma apps. Both modalities can be used in teledermatology, extending expert dermatological advice to patients in regional and rural areas where in-person dermatology appointments range from limited to non-existent. The images, acquired either by the patient via mobile teledermoscopy or by a melanographer operating a 3D total body imager, can be transmitted to a city-based dermatologist for review and management recommendations.
Precision prevention of melanoma is a promising approach to dealing with two problems in melanoma diagnosis: overdiagnosis and missed diagnoses. Dermatologists are familiar with the problem of missed diagnoses, especially in patients with many naevi. However, overdiagnosis is also increasingly recognised as a problem in melanoma treatment, with as many as 58% of melanomas in Australia over diagnosed. These are true but indolent cancers that would not have caused illness in the patient’s lifetime, and they are currently undistinguishable from thin melanomas with invasive potential, where early excision is usually curative2. Although excisions of over diagnosed melanomas are currently necessary for patient and clinician peace of mind, they are an extra burden of the health care system and come with undesirable side effects such as scarring, infection, and psychological distress.
References
- Smithers BM, Dunn J and Soyer HP. Whither melanoma in Australia? The Medical journal of Australia 2017; 207: 330-331. 2017/10/13. DOI: 10.5694/mja17.00740.
- Glasziou PP, Jones MA, Pathirana T, et al. Estimating the magnitude of cancer overdiagnosis in Australia. The Medical journal of Australia 2020; 212: 163-168. 2019/12/21. DOI: 10.5694/mja2.50455.
- Lee KJ, Betz-Stablein B, Stark MS, Janda M, McInerney-Leo AM, Caffery LJ, Gillespie N, Yanes T, Soyer HP. The Future of Precision Prevention for Advanced Melanoma. Front Med (Lausanne). 2022 Jan 17;8:818096. doi: 10.3389/fmed.2021.818096. PMID: 35111789; PMCID: PMC8801740