Global Dermatology
Contributions from WCD2023 Ambassadors

Collection of articles about dermatology from all over the world. Dermatology beyond borders.
Dermatology in the United States during COVID-19
The COVID-19 pandemic began in early 2020, and since then, it has devastated the lives of millions of people across the globe. It is truly a defining moment of world history that we should do our best to never forget.
Yet, out of the tragedy, some positives have arisen. For starters, dermatologists have been able to completely revolutionize how they incorporate telehealth into their practices. Prior to the pandemic, there were many legal issues surrounding telederm in the U.S., with many dermatologists prohibited from practicing across state lines. When the pandemic hit and state legislatures enacted laws in response, many of those legal restrictions were eased or lifted entirely, which vastly increased the potential reach of dermatologic care, and many practices across the country took the pandemic as an opportunity to upgrade and expand their own telehealth services.
We’ve also seen major innovations in treatments, which have gone far beyond their capabilities from the past and have completely changed the way dermatologists treat some conditions. Within the past few months, JAK inhibitors have been proven effective and given FDA approval to treat a variety of conditions, including vitiligo, alopecia, and atopic dermatitis, while tapinarof and roflumilast creams have been approved for treating psoriasis, offering effective topical relief to many patients.
As life-changing as some of these advancements have been, it’s important to realize they won’t be as effective as they can be unless we ensure that doctors know about them. As President of the American Academy of Dermatology, I take great pride in how quickly and efficiently our organization shares important industry news with our members.
Our mission is to deliver gold-standard education, information, and data so that our members have the most up-to-date information on clinical advances and relevant treatment, and we meet this goal in a variety of different ways. The AAD circulates various publications, including DermWorld, the Journal of the American Academy of Dermatology, and the Dialogues in Dermatology podcast series, that receive thousands of views and listens per month from members. DermWorld and JAAD each have an international edition with which many of you around the world may be familiar.
Back in the United States, the Academy is the foremost collective voice of dermatology, and in that role, we advocate effectively on behalf of our members and dermatology to the public and to policymakers across all levels and branches of government. We have a history of helping enact meaningful changes; at the moment we are working hard to make sure that dermatologists in the United States continue to be paid fairly for the services we provide to Medicare patients. We’re also striving to remove barriers like step therapy and prior authorization that threaten patients’ access to treatments and care.
The past two and a half years have been an extremely difficult time for everyone around the world, and dermatologists are not immune from that struggle. But, thanks to the expansion of telehealth, the innovations in treatment, and the dedicated work of the AAD, I am confident that we will make it through to the other side stronger than we were before.
I look forward to seeing many of you in Singapore in July!

Subungual frictional hematoma
Correspondence to: Patricia Chang, MD, pchang2622@gmail.com
Dra. Patricia Chang declares: Non-Financial Support and Non-Conflict of interest.
Key words: subungual frictional hematoma, micro trauma
CLINICAL CASE
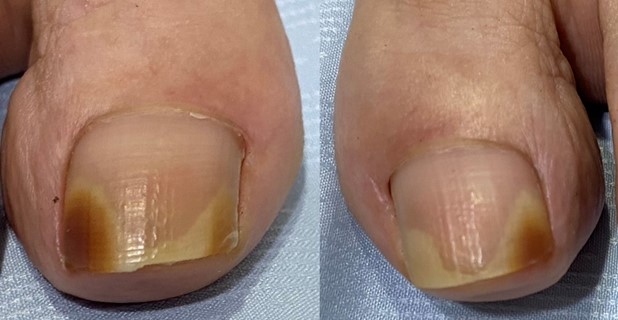
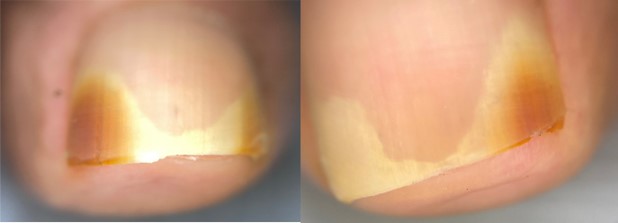
A 73 -years-old female patient presented with alterations of both big toenails, which showed onycholysis and brown discoloration (Fig.1,2), dermatoscopy reveals onycholysis and dyschromia also (Fig.3). The rest of the physical exam was normal.
Her condition started 4 years ago with discoloration of her both great toenails without any symptoms. She was treated with different antifungals drugs during these four years and doctors. Her last doctor sent to me for an onychological opinion.
Family history negative and relevant personal history: diabetes mellitus since five years ago controlled with metformin 1000 mg daily.
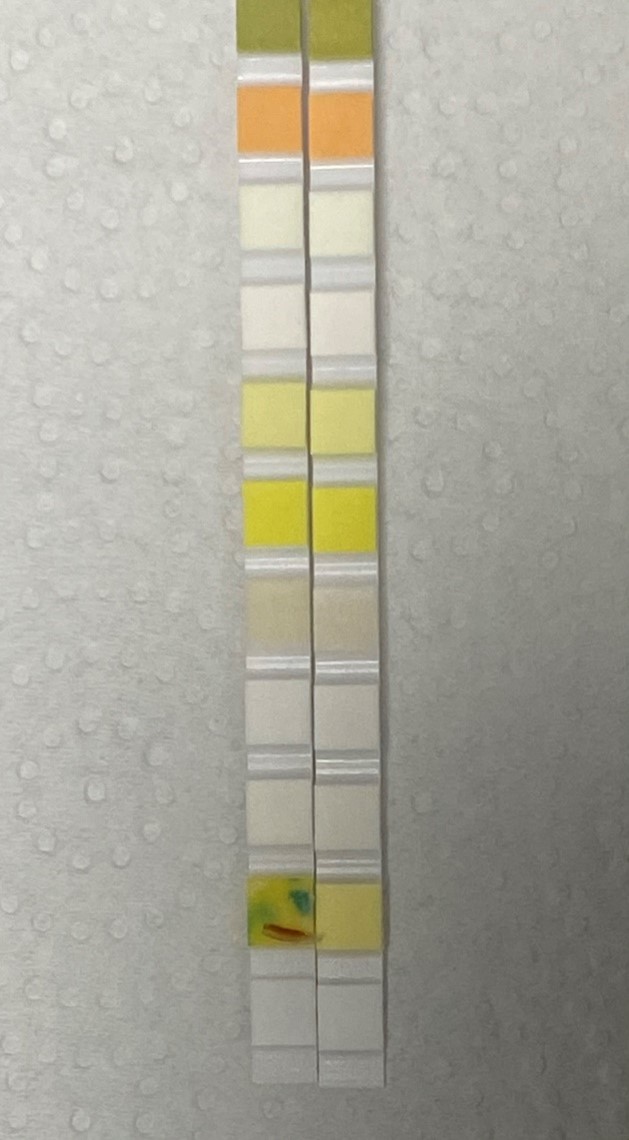
With these ungual signs and the symmetry of the bilateral lesions, a subungual frictional hematoma was diagnosed. A urinary strips screening test to evaluate blood was performed, KOH and fungus culture was done, the urinary strip for blood was positive in both big toenails (Fig.4) KOH and fungus culture was negative. The final diagnosis was subungual frictional hematoma.
Questioning the patient again to find the cause of her frictional hematoma, she recalled that since that time she has been using insoles prescribed by her doctor.
Discussion
A hematoma is a collection of blood at any part of the body caused by different factors. In the nail, the best-known hematomas are the ones produced by major trauma with injury to subungual structures such as the nail bed and matrix. Besides these, hematomas may be secondary to systemic diseases, infectious, tumoral, congenital, iatrogenic conditions and medications that do not only affect the nail bed, but also the folds and cuticle. Heavy trauma is a major cause of ungual dyschromia, above all in feet, secondary to strong blows like in athletes who practice football, climbing, skiing, running, tennis, and others Rubbing is a special type of trauma, hence the term of frictional hematoma, which is in fact a traumiterative hematoma. It can be considered as a type of occupational disorder in people that use steel tipped shoes at the job. It is observed where chronic rubbing with a certain amount of pressure occurs, but toes are by far the most common to be involved. Tennis toe, ski-boot toes, surfboard toes, narrow tipped boots, tight and high heels shoes, may be due to chronic friction or chronic pressure (1)
The hematoma due to more or less heavy trauma are called acute hematomas and it´s treatment is the trephination and the chronic is due to repeated minor trauma such as friction and for its treatment it´s important find the cause. The frictional hematomas are often oval with their long axis in longitudinal direction; most are located on the lateral aspect of the big toenail as a result of rubbing of the first to the second toe (2)
Subungual hematomas of the nails are common it could be cause by major and minor trauma predominantly on the big toe, the different toe deformity (overlapping toes) predispose to have subungual frictional hematomas (3)
Some authors have reported 2 cases of foot subungual frictional hematoma in 2 male patients associated in one of them with steel toe shoes due to their occupation and in another patient due to the use of tight shoes (1)
Clinically, it can manifest as a blackish brown, brown or blackish subungual -nail dyschromia and onycholysis that can affect the nail partially, totally or longitudinally according to the friction or pressure that the shoe makes to the nail. The diagnosis is easy using the dermatoscope and a test strip for blood as used for the diagnosis of hematuria or fecal blood, the simple and fast method which consists of placing nail fragments on a urine strip, then adding a drop of water and after 60 seconds observe a green coloration, which indicates that it is a positive reaction for blood, being a simple and easy method to used (5)

References
- Chang P, Haneke E, Rodas AC Hematomas del Aparato Ungueal Dermatología Cosmética Médica y Quirúrgica 2009; 7(3):196-201
- Haneke E. Nail Specific Conditions en: Histopathology of the nail. Onychopatology. Taylor & Francis B Group USA: 146-147
- Chang P Hematoma Friccional secundario a Dedos Traslapados Dermatología Cosmética Médico Quirúrgica 2009; 7(2): 138-141
- Chang P, Haneke E, Borjas Leiva CA, Pellecer D. Hematoma friccional subungueal. Dermatologia CMQ 2,012; 10(1).48-50
- Chang P. Subungual frictional hematoma due to overriding toe. N Dermatol Online. 2011; 2(3): 151-152