Contributions from WCD2023 Ambassadors
Global Dermatology

Collection of articles about dermatology from all over the world. A dermatology beyond borders.

WCD Ambassador, Italy
Gaetano Licata MD1, Giuseppe Argenziano MD, PhD.1
1Dermatology Unit, Department of Mental and Physical Health and Preventive medicine, University of Campania Luigi Vanvitelli Naples, Italy
Diagnosis and management of melanoma of the scalp
Cutaneous melanoma is a public health issue, particularly in light-skinned populations. The head and neck region is of particular interest, despite accounting for only 9.0% of the total body surface, it harbours 20% of melanoma cases1. Scalp melanoma (SM) represents 35% of cases of head and neck melanomas and is accountable for 5% of all melanomas2. Data from the literature show that SMs carry the highest mortality rates, with a 10-year survival rate of 60% which lead them to be named as the “invisible killer”. The worst clinical behaviour has been attributed to several factors including delayed diagnosis due to poor visibility of the area (hair coverage); a higher proportion of melanomas with rapid vertical growth, such as nodular and desmoplastic melanomas; a more aggressive nature related to anatomical features such as abundant lymphatic and blood drainage and finally the difficulty of obtaining adequate surgical margins3. This knowledge indicates that there is a need to improve the early detection of melanoma on this specific location. SMs are more common in the elderly than in young population, and they occur six times more frequently in men than in women. This is probably related to the higher incidence of androgenetic alopecia and a higher cumulative and intermittent ultraviolet damage on the scalp. Histologically, SM is a heterogenous group of neoplasms including different histological subtypes, including lentigo maligna melanoma (LMM) and desmoplastic melanoma, superficial spreading and nodular melanoma.

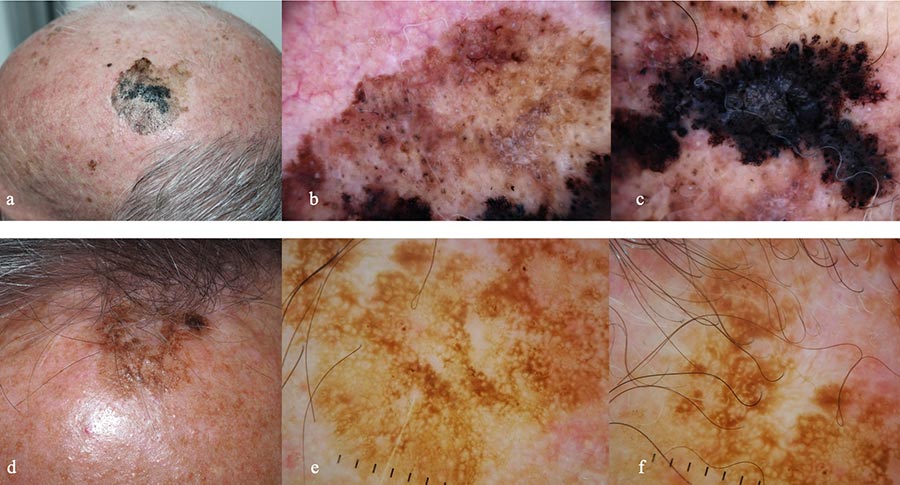
On dermoscopy, thin melanomas tend to display an atypical network or pseudo-network and regression in dermoscopy, furthermore blue-white veil, irregular pigmented blotches and an unspecific pattern are most commonly detected in thick lesions (fig 1). On reflectance confocal microscopy (RCM), the most frequent pattern is irregular meshwork, but also ringed and disarranged pattern have been described. Differential diagnosis includes benign solar lentigo, actinic keratoses, lichen planus like keratosis, all characterized by a brown pseudonetwork (fig 2). Scalp nevi and blue nevi can be included in differential diagnosis of SSM. When discussing specifically lesions of the head and neck, during childhood nevi tend to be flat and show benign features such as cobblestone pattern, homogeneous pattern and typical pigment network. Targetoid or “crown” appearance have also been described. Afterwards, with aging, these lesions are likely to become dermic and less pigmented4. Blue nevi show a preference for scalp location, in dermoscopy they are characterized by structureless blue pigmentation. All suspicious lesions should be biopsied, therefore, an excisional biopsy with 2 mm margins is usually the best option. However, when lesions are extensive or excisional biopsy is not possible, incisional or punch biopsy are viable alternative options for establishing the diagnosis5. The diagnosis of scalp melanoma is usually possible on clinical examination; however, a definitive diagnosis is confirmed on histopathological examination only. Dermoscopy and RCM can be very useful tools in making a clinically accurate diagnosis and eventually guide the selection of the best area to biopsy in case of large and extensive lesions and leading patents’ management.
References
- Dabouz F, Barbe C, Lesage C, Le Clainche A, Arnoult G, Hibon E, Bernard P, Grange F. Clinical and histological features of head and neck melanoma: a population-based study in France. Br J Dermatol. 2015 Mar;172(3):707-15. doi: 10.1111/bjd.13489. Epub 2015 Feb 11.
- de Giorgi V, Rossari S, Gori A, Grazzini M, Savarese I, Crocetti E, Cervadoro E, Massi D. The prognostic impact of the anatomical sites in the ‘head and neck melanoma’: scalp versus face and neck. Melanoma Res. 2012 Oct;22(5):402-5. doi: 10.1097/CMR.0b013e3283577b96.
- Porto AC, Pinto Blumetti T, Oliveira Santos Filho IDA, Calsavara VF, Duprat Neto JP, Tavoloni Braga JC. Primary cutaneous melanoma of the scalp: Patterns of clinical, histological and epidemiological characteristics in Brazil. PLoS One. 2020 Oct 23;15(10):e0240864. doi: 10.1371/journal.pone.0240864.
- Shitara D, Nascimento M, Ishioka P, Carrera C, Alós L, Malvehy J, Puig S. Dermoscopy of Naevus-associated Melanomas. Acta Derm Venereol. 2015 Jul;95(6):671-5. doi: 10.2340/00015555-2009. PMID: 25394499.
- Munsch C, Lauwers-Cances V, Lamant L, et al.. Breslow thickness, Clark index and ulceration are associated with sentinel lymph node metastasis in melanoma patients: a cohort analysis of 612 patients. Dermatology. 2014;229(3):183-189.25171688 Crossref, Medline, Google Scholar.
Figure Legend
Figure 1: Nevus associated melanoma arising on the scalp in a 55-year old man with androgenic alopecia. a. Clinically, asymmetrically pigmented macule is visible B. In dermoscopy, blue-white veil.
Figure 2: Lentigo maligna melanoma on the scalp of a 78-year old man with androgenic alopecia and solar lentigo on the scalp of a 81-year old man. a. Clinical appearance of the LMM. A large macule, variegated in color from light to dark brown to black with defined borders. In the background, signs of extensive sun-damage. b. Dermoscopy showing a brown pseudo network with grayish circles around follicular openings and white streaks. c. Dermoscopy of the hyperpigmented part, with obliteration of follicular openings, blue -white veil and irregular dots.
d. Clinical appearance of a solar lentigo: a brown macule with a hyperkeratotic component. e.and f. Dermoscopy showing a light brown pseudo network with evident follicular openings.
All correspondence to:
Giuseppe Argenziano, MD
Dermatology Unit, University of Campania “Luigi Vanvitelli”
Via Sergio Pansini, 5-80131 Napoli, Italy
Phone: +39.081.5666828; Fax: +39.081.546.87.59; E-mail: g.argenziano@gmail.com

WCD Ambassador, Malaysia
Regional Scientific Meeting of Paediatric Dermatology (RSMPD) 2021
The Dermatological Society of Malaysia hosted the 10th Regional Scientific Meeting of Paediatric Dermatology (RSMPD) in conjunction with the 46th Malaysian Annual Dermatological Conference from 29th July to 1st August 2021. The conference, with the theme “New Advances on Paediatric Dermatology”, was held virtually due to travel restrictions worldwide.
A total of 785 delegates from all over the world participated in the conference. The organising committee, chaired by Dr Sabeera Begum, drew up an academically stimulating scientific programme targeting not only dermatologists, paediatricians and general practitioners but also allied health professionals as well.
The programme consisted of two parallel sessions for paediatricians and dermatologists respectively, highlighting the basics and new dimensions of Paediatric Dermatology. The conference kicked off with the pre-congress event featuring “Masterclass and Advanced class on Atopic Dermatitis” which focused on basic knowledge for the junior doctors and “Paediatric Dermatology Clinicopathological Conference (CPC)” which was targeted at the pathologists and dermatologists.
The conference was officiated by the Director-General, Ministry of Health Malaysia, Tan Sri Dato’ Seri Dr Noor Hisham Abdullah. There were a total of 3 plenaries and 14 symposiums and 66 lectures. We were privileged to have with us a panel of esteemed experts in the field of paediatric dermatology, both internationally and locally, to share their experience and expertise.
Our 3 keynote speakers were Professor Amy Paller from USA, Professor John McGrath from UK and Professor John Su from Australia. Others distinguished speakers hailed from Singapore, Thailand, Philippines, Indonesia, Hong Kong, India, Taiwan, New Zealand, Germany and Canada. Our local speakers featured a number of young and talented doctors who did us proud.
We received a total of 107 good quality studies, comprising 16 oral presentations and 91 e-posters presentations. Prizes were given out to the top 3 presenters for both the oral and poster categories for both paediatric and adult dermatology.
The conference would not be possible without the support of our biomedical industry partners who contributed by putting up virtual exhibition booths.
We received many positive feedback and appreciation from our delegates reflecting a successful RSMPD 2021. Kudos to Dr Sabeera and her team for a job well done!



WCD Ambassador, Australia
The importance of Skin of Colour dermatology
It was August 2008. Obama was campaigning for his Presidency and the world had plunged into a global financial crisis. I moved from Melbourne, Australia to the National Skin Centre (NSC) in Singapore to undertake a six-month dermatology training stint. Australia had long had a wonderful partnership with Singapore whereby two dermatology registrars spend 6months each year at NSC during their four-year training program. I had no idea that this six-month stint was going to inspire me to delve into the world of pigmentary disorders, challenge me to champion change in the area of skin of colour dermatology and advocate for cultural diversity in healthcare.
As our global family becomes even more culturally diverse with more global movement of people across borders, dermatologists practicing in any corner of the globe are likely to encounter patients from different ethnic and cultural backgrounds. There is no denying that dermatology has no boundaries in 2021. Wherever you practice, understanding the prevention, presentation, treatment and complications of hair, skin and nail issues in skin of colour is more important than ever before. And tailoring your communication and treatment plans to suit the cultural context should not be underestimated.
Our research in 2016/2017 demonstrated a lack of confidence among Australian dermatology trainees and dermatologists in diagnosing and managing conditions in skin of colour. Over 80% of dermatologists were not confident in managing common cosmetic issues in skin of colour and over 80% would have liked more training and education in skin of colour dermatology during their training. The sentiments were echoed by Australian dermatology trainees. Our study findings were not unique. Research well before ours lead by skin of colour experts in the USA and UK revealed similar knowledge gaps in this area of dermatology.
I am proud that the Australasian College of Dermatologists have recognised the importance of this area of dermatology and have added a module on skin of colour into the dermatology training curriculum. We further revised and expanded the module again last year which was another step in the right direction.
Prevention, pathogenesis, morphology, response to therapy and complications all different in different skin types. We all need to learn more about dermatology beyond our borders today so we can better help those who seek our care tomorrow. The World Congress of Dermatology meeting in Singapore will give us this opportunity. I look forward to seeing you there.
1. Australian dermatologists’ perspective on skin of colour: Results of a national survey.
Rodrigues MA, Ross AL, Gilmore S, Daniel BS.Australas J Dermatol. 2018 Feb;59(1):e23-e30. doi: 10.1111/ajd.12556. Epub 2016 Dec 9.
2. Australian trainee dermatologists’ opinions on skin of colour education: Does it reflect changing demographics of the population? Wee E, Gilmore S, Rodrigues M. Australas J Dermatol. 2018 Aug;59(3):e239-e240. doi: 10.1111/ajd.12693. Epub 2017 Aug 3.
3. Dermatology training in the U.K.: does it reflect the changing demographics of our population?
Salam A, Dadzie OE.Br J Dermatol. 2013 Dec;169(6):1360-2.